

The standard radiographic projections for a suspected talar neck or body fracture include an anteroposterior (AP) and lateral view of the ankle. The various complications are avascular necrosis, malunion, infections, late osteoarthritis, and ankylosis of subtalar joint. Clinical outcomes depend on the severity of the initial injury and the quality of reduction and internal fixation. Sometimes, a dual approach with a malleolar osteotomy is necessary for articular restoration. Surgery is indicated in most of the cases, and different approaches have been described. Splinting, followed by short leg casting for 6 weeks until fracture union should be undertaken. Indications for nonoperative management are seldom indicated and are few as in nonambulatory patients, or in with multiple comorbidities who are not able to tolerate surgery. Optimal treatment relies on an accurate understanding of the injury and the goals of treatment are the restoration of articular surface and axial alignment. Differentiating talar neck from body fractures is important.
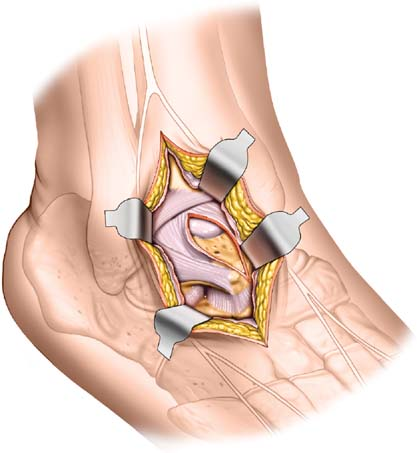

The initial evaluation should be done with foot, and ankle radiographs and computed tomography is often done to analyze the extent of the fracture, displacement, intraarticular extension, comminution, and associated fractures. Associated neurovascular injury of the foot should be carefully examined. Clinically, talar body fractures present with soft tissue swelling, hematoma, deformity, and restriction of motion. Great care is necessary for diagnosing and treating these injuries. Axial compression with supination or pronation is the common mechanism of injury. They occur as a result of high-velocity trauma and are therefore associated with considerable soft tissue damage. The relative infrequency of this injury limits the number of studies available to guide treatment. The integrity of the talus is essential for the normal function of the ankle, subtalar, and midtarsal joints. Fractures of talar body are uncommon injuries often associated with fractures of other long bones and in polytraumatized patients.


 0 kommentar(er)
0 kommentar(er)
